Endoscopic Mucosal Resection and Endoscopic Submucosal Dissection: Minimally Invasive Techniques for Resecting GI Mucosal Tumors
Major advances in the development of endoscopic devices and techniques over the past fifteen years have introduced endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) as standard of care for the safe and effective removal and/or definitive staging of mucosal lesions of the esophagus, stomach, duodenum and colon, often eliminating major surgery as first-line management. Gastroenterologists at Penn State Health Milton S. Hershey Medical Center including Abraham Mathew, MD, Matthew Moyer, MD, and Charles Dye, MD, have become leading clinicians and active researchers in these techniques, performing several hundred EMR procedures annually. Mathew explains, “EMR is the more widely used of these techniques for removal of smaller tumors or lesions [<2.5 cm]. With EMR, normal saline or hydroxy propyl methylcellulose, dilute epinephrine and methylene blue are injected into key areas of the submucosal space beneath the tumor, strategically positioning the tumor and separating it from the bowel wall; the tumor can then be resected with less risk of thermal or mechanical damage to the muscularis propria. With ESD, a more aggressive technique for removal of larger, more invasive tumors, the surgeon uses specialized devices to tunnel into the submucosal plane to dissect the tumor en block. Incisions are closed endoscopically with sutures or clips.”
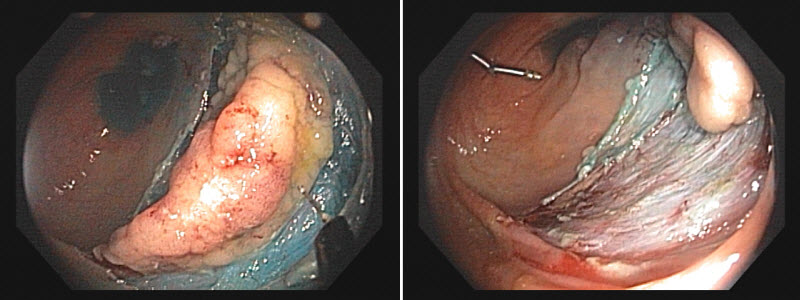
A colon mass lesion in the process of being resected by ESD.
Moyer notes that the benefits of EMR and ESD outweigh the risks when performed in a high volume center with an appropriate team who have the correct equipment and procedure volume; however, complications can occur and should be explained to the patient. “Complications include bleeding, which occurs in five to ten percent of cases, and a lower risk of perforation (1 percent EMR, 2 to 5 percent ESD). Incomplete removal of abnormal tissue is a longer-term complication with EMR (between 1 and 11 percent) and ESD (1 percent).”
Risks are potentially greater in patients with lesions unsuccessfully removed during a screening procedure. This team strongly advises referring physicians to avoid attempting to remove any lesion that is not felt to be appropriate for complete removal during the screening procedure. Dye explains, “With failed attempts at lesion removal, the resulting inflammatory reaction can adhere remaining abnormal tissue to the muscularis propria, making subsequent endoscopic removal difficult and raising the potential for major surgery.” Referring physicians are advised to mark the target lesion, obtain a biopsy from the periphery if necessary, and refer the patient to tertiary care so that removal is complete and risks are minimized.
Patients typically undergo routine surveillance endoscopy at three or six months and one year after. Mathew notes, “Minimally invasive procedures like EMR and ESD can make a real difference in the life of a patient. They can return to normal activities usually the next day with a very low risk of any complication or lesion recurrence.”
Indications for EMR or ESD
- Mucosal lesions of the esophagus (cancerous or potentially cancerous) including lesions within Barrett’s esophagus and short-segment Barrett’s esophagus with dysplasia
- Gastric mucosal lesions
- Duodenal lesions, including ampullary lesions requiring ERCP-assisted ampullectomy
- Adenomatous colon and rectal lesions not amendable to safe or complete removal during screening colonoscopy
- Limited gastric and rectal carcinoid tumors
- Select submucosal lesions

Charles E. Dye, MD
Associate Professor of Medicine, Medical Director, Endoscopy Center
Penn State Gastroenterology
Phone: 717-531-1441
Email: cdye@pennstatehealth.psu.edu
Fellowship: Therapeutic Endoscopy, University of Chicago Medical Center; Gastroenterology, University of Chicago Medical Center
Residency: Internal Medicine, University of Chicago Medical Center
Medical School: Penn State College of Medicine
Connect with Penn State Health Gastroenterology and Hepatology on Doximity

Abraham Mathew, MD
Professor of Medicine
Phone: 717-531-1441
Email: amathew@pennstatehealth.psu.edu
Fellowship: Gastroenterology, Penn State Health Milton S. Hershey Medical Center
Residency: Internal Medicine, Abington Memorial Hospital
Medical School: Mahatma Gandhi University
Connect with Penn State Health Gastroenterology and Hepatology on Doximity

Matthew T. Moyer, MD, MS
Professor, Department of Medicine, Division of Gastroenterology and Hepatology, Penn State Cancer Institute
Phone: 717-531-4950
Email: mmoyer@pennstatehealth.psu.edu
Fellowship: Gastroenterology, Penn State Health Milton S. Hershey Medical Center, Hershey, Pa.
Residency: Internal Medicine, Penn State Health Milton S. Hershey Medical Center, Hershey, Pa.
Medical School: Penn State College of Medicine, Hershey, Pa.
Connect with Matthew T. Moyer, MD, MS, on Doximity
